CPR
(CARDIOPULMONARY
RESUSCITATION)
NOTE: DO NOT PERFORM ANY MEDICAL PROCEDURE WITHOUT TRAINING OR CERTIFICATION]
Despite
technological advances and new scientific discoveries, heart disease remains
the number one cause of death globally, with 17.3 million deaths per year.
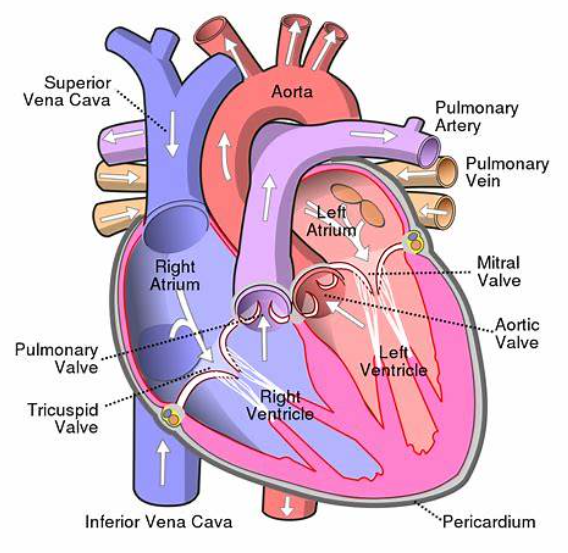
HEART
The heart consists of four chambers,
the right and left atria (singular: atrium)
and the right and left ventricles. The atria are located above the ventricles, as can be seen in the
above diagram. The heart is a
muscular organ supplied by the coronary arteries. It is located below your
breastbone (sternum) and, in an adult, is approximately the size of your fist.
The heart pumps blood that has been deoxygenated after supplying the body’s tissues
into the
lungs, and when that blood
has been oxygenated again in the lungs, it exits the lungs to the left.
side of the heart, where it is pumped out into the body once again,
to provide oxygen to all your vital organs.
Your body has about 5 liters
of blood, which circulate through
this system approximately 3 times per minute.
What is known as the cardiovascular system is composed
of the heart, arteries, capillaries, and veins.
LUNGS
Your
lungs are spongy, air-filled sacs, with one lung located on either side of the
chest. The trachea, which is sometimes called the windpipe,
conducts air down into the lungs through
the
bronchi,
which are smaller tubular branches. The bronchi then divide into smaller and
smaller tubules called bronchioles. Air is exchanged in the alveoli,
which are tiny sacs that allow oxygen and carbon dioxide to move between
the lungs and the bloodstream via tiny capillaries.
Your lungs take in oxygen to supply your body’s organs
and tissues. They release
carbon dioxide, a waste product, into the atmosphere when you exhale.
Room
air at regular atmospheric pressure contains 21% oxygen. Our bodies utilize
approximately 4-6% of that oxygen and release
about 16-17% back into the atmosphere, along with carbon dioxide, when we exhale.
This 16-17% that we exhale can provide just enough oxygen to sustain someone in
cardiac arrest, at least for a short time.
BRAIN
Your brain needs a constant supply
of oxygen. Without
oxygen, brain cells
begin to die in 4 to 6 minutes.
On average, the brain weighs three pounds,
and uses a whopping 20% of the body’s oxygen!
The medulla
is located in the brain stem and controls automatic bodily functions, including consciousness and respiratory
and cardiovascular function.
BODY CELLS
All of the body’s tissues
are made up of cells.
All cells require oxygen to carry out their normal functions. They also require
nutrients. Oxygen deprivation,
or hypoxia, will cause cells to die within a few short minutes.
The body’s cells
use oxygen and produce carbon
dioxide as a waste product. Carbon dioxide must be
eliminated via the lungs through ventilation.
Red blood cells transport oxygen throughout the body.
CARDIOVASCULAR DISEASE
As
mentioned previously, cardiovascular disease is the number one cause of death
worldwide. While it is important to learn
what to do when cardiovascular disease leads to a heart attack or stroke, it is equally as important, if
not more so, to understand how to prevent cardiovascular disease from occurring
in the first place.
There are numerous factors
that can increase
an individual’s risk of heart attack. Some of these factors can be controlled
(modifiable risk factors), while others cannot (non-modifiable risk factors.
Modifiable risk factors, or factors that can be controlled to a certain degree by an individual, include:
a) cigarette smoking
b) hypertension
c)obesity
d) sedentary lifestyle (lack of exercise)
e) high cholesterol
f) high blood sugar (as in diabetes)
g) poor diet (diet high in sugar, fat)
h) stress
Non-modifiable risk factors, or risk factors that individuals cannot change, includes:
a) age
b) sex
c) genetics/hereditary factors (i.e. hereditary high cholesterol or hyperlipidemia)
d) race (i.e., certain groups may be at higher risk for hypertension, or high blood pressure)
Atherosclerosis, or hardening of the arteries, is a condition caused by the building up of plaque inside the body’s arteries, the large blood vessels that carry blood away from the heart to the body’s organs. Plaque is composed of fatty substances, cholesterol, fibrin (a clotting substance in the blood), calcium and cellular waste products.
When plaque builds up, it can partially or totally block the flow of blood through an artery in the brain (which causes stroke), the heart (which causes a heart attack), the kidneys, the arms, the legs and other vital areas. Plaque may break off to block an artery, or a blood clot (thrombus) may form on the surface of the plaque- either of these two circumstances can lead to a heart attack or stroke.
HEART ATTAC
A heart attack of ten presents with one or more symptoms:
a) Chest tightness, pressure, or discomfort
b) Nausea
c) Sweating
d) Shortness of breath
e) Fatigue
f) Weakness
g) Pain in the jaw or arm
h) Pale color of the skin
Women and people with diabetes often present with atypical symptoms, such as nausea
and vomiting or back pain. About one-third of patients report no chest
pain at all.
WHAT CAN WE DO?
a) Recognize the symptoms and signs of a heart attack.
b) Call for medical/professional help.
c) Don’t let the patient drive him or herself to the hospital
d) Keep the patient calm and seated in a position that is comfortable.
e) Offer 1 adult aspirin or 2 baby aspirin- aspirin should be chewed before swallowing to speed absorption (Note: do not give if the patient has already taken aspirin or if the patient has an allergy to aspirin)
f) Be prepared to start CPR if it becomes necessary
STROKE
You should suspect a stroke if a patient presents with:
a) Severe headache with no known cause
b) Numbness or weakness of the face, arm or leg on one side of the body
c) Drooping eyelid or mouth on one side
d) Confusion or trouble understanding
e) Difficulty speaking /slurred speech
f) Loss of balance or coordination
g) Dizziness
h) Trouble with vision/blurred, double vision or loss of vision in one eye.
WHAT CAN WE DO?
a) Know the signs and symptoms of a stroke
b) Call for medical/professional help. Don't give the patient food or drink.
c) Keep the patient calm and quiet
d) Monitor the patient
e) Be prepared to begin CPR if it becomes necessary
A stroke is caused by one of two mechanisms: it can be caused by a ruptured blood vessel in the brain (called a hemorrhagic stroke) or by a blockage in one of the arteries that causes loss of blood flow and oxygen to a part of the brain (called an ischemic stroke). Ischemic strokes are more common.
Remember that “Time is
brain,” and act quickly. Stroke is the 3rd leading cause of death in
the world.
STARTING CPR
HIGH QUALIYT CPR:
1) Compression rate of 100- 120 beats per minute on victims of all ages.
2) Compression depth of AT LEAST 5 cm maximum in adults
3) Allow the chest to completely expand (recoil) after each compression (do not lean on the chest between compressions)
4) Not interrupting CPR
5) Avoiding excessive ventilations
6) Above all else, PUSH HARD ENOUGH AND FAST
a) Since many responders and even professionals are unable to feel or palpate a pulse quickly, the recommendation is to feel for a pulse for not more than 10 seconds. If you can’t feel a pulse or you’re not sure you can feel a pulse-start CPR.
b) It has been recognized that health care professionals should call for assistance when they come upon an unconscious victim, but they may also simultaneously assess breathing and check for a pulse before fully activating the emergency response system. This may encourage efficiency in assessment and response, rather than following a step- by-step response.
c) Rescuers should provide 2 breaths and then 30 compressions continuously.
NOTE:
DO NOT PERFORM ANY MEDICAL PROCEDURE WITHOUT TRAINING OR CERTIFICATION]
CHEST COMPRESSIONS
Chest compressions are the most important component of CPR. Chest compressions are an attempt to mimic the normal activity of the heart. When a rescuer presses down on a victim’s chest, blood is forced out of the heart and into the arteries. When pressure on the chest is released, blood is allowed to return to the heart.
A small amount of oxygen will be present in the bloodstream for several minutes after the heart ceases to beat, just enough to keep the brain alive. Compressions can keep vital organs functioning until higher level care is available.
To perform compressions on an adult, place the heel of your non-dominant hand on the victim’s chest between the nipples.
Then place your other hand on top of the first and interlace your fingers heel of your hand should be pressing on the bottom two-thirds of the sternum, avoiding the xiphoid process (the small bony prominence at the very bottom of the sternum (breastbone).
You should be as close to the victim’s side as possible, with your knees against the victim’s side (this will help prevent back injury). Lock your elbows and press down hard, depressing the sternum at least 2 inches (5 cm).
Your shoulders should be positioned directly over your hands in a straight line
Push hard and fast 100 to 120 times per
minute, counting out loud as you do so. It’s important that you allow the chest to recoil (return to its normal, relaxed position) in between compressions. If you do not allow the chest to recoil, the heart will not fill completely, which means that less blood (and therefore oxygen) will be pumped out of the heart to vital organs with the next compression.
Performing compressions is exhausting. Most people find that they become very tired after providing compressions for 2 or 3 minutes. When a person performing compressions becomes fatigued, there is a tendency to compress less firmly and more.
slowly, for this reason, it is recommended that rescuers trade off doing compressions every 2 minutes to prevent fatigue and optimize the quality of compressions. If you are alone, you will have to do the best you can- keep performing compressions until help arrives or you are physically so exhausted that you cannot continue.
ONLY ONE RESCUER
If you are alone and come across an individual who is down, follow the steps below. If someone else is in the area to assist, use the ‘Two Rescuer’ sequence.
SAFETY:
If you come upon an individual who may need CPR, look around and make sure you and the victim are in a safe place.
For example, if the victim is in water or on a road, try to move the victim to a safer area. If you are in a safe area, do not try to move the victim as he/she may have other injuries (i.e., to the head or neck) that you cannot see. Simply roll him over onto his back.
Make sure the victim is on a firm surface, in
case compressions are needed.
ASSESS THE VICTEM:
To quickly assess the victim, shake his shoulder and yell at him.
Check for breathing. If he/she
is not breathing, or is not breathing normally (i.e., only gasping), you must
summon help. Note: Agonal breathing is
breathing that is very slow, shallow and/or gasping.
Agonal breathing is a sign that the victim is dying. It is important not to mistake
agonal breathing for normal breathing!
BEGIN CPR:
1. Check for a
pulse on the side of the neck. Feel
for a pulse for at least 5 seconds but NO MORE
THAN 10 seconds.
To check for a carotid
pulse, slide 2 or 3 fingers into the groove between the windpipe and the neck
muscles at the side of the neck.
2. If there is no pulse (or if
you are unsure
if there is a pulse),
begin CPR starting
with chest compressions.
Provide 30 chest compressions, followed by two breaths.
3. NOTE: If
you are not comfortable giving rescue breathing and/or you do not have a mask
available, do ‘Compression Only’ CPR.
a. Use the heel of one hand on the lower half of the breastbone in the middle of
the chest.
place the other hand on top of the first
hand.
c. Straighten your arms and lock your elbows so that your body weight
is over your hands.
d. The most
important part of CPR is to remember to push HARD and FAST. Each compression should be AT LEAST 5 cm deep, and the rate should be 100-120
compressions per minute.
e. Be sure to let up on the pressure
on the sternum after each compression (chest recoil) so the chest can re-expand, and blood can flow back into the heart. The
purpose of CPR is to help the blood flow through the heart and into the rest of
the vital organs; if you allow the chest to re-expand, more blood will flow
into the heart and will be available to deliver to the rest of the body.
f. Count out loud as you do compressions. When you have done 30 compressions,
try to open the victim’s airway by doing a head tilt/chin lift. Note that if
you are doing ‘Compressions Only’ CPR, you can skip this step.
i. With your non-dominant hand, push on the victim’s
forehead to tilt the
head back.
ii. With your dominant hand, place your fingers under the bony part of the
lower jaw and gently lift the jaw to bring the chin forward. Be sure you lift up on the bony part of
the jaw and not the soft tissue under the jaw, so you don’t block the victim’s airway. Do not use your thumb to lift
the jaw. Allow the victim’s mouth to remain slightly open.
iii. If you think the person’s
neck may be injured, avoid the
head tilt/chin lift. Use the jaw
thrust maneuver if you have been trained to do so.
g. If you have
a barrier device to use between your mouth and the victim’s face, use it.
Although the risk of infection from performing CPR is very, very low, it is
expected that healthcare workers use a barrier device when providing CPR. This
includes the use of face masks or bag-mask devices
(see next section).
Give each breath slowly –
each breath should last one second. Make
sure the chest rises with each breath. Repeat,
giving a second breath.
h. Start another
cycle of chest compressions. Remember,
push HARD and FAST.
Alternate chest compressions (30) and giving breaths (2) until help arrives.
AIRWAY & BREATHING
Face masks
provide a barrier
between the rescuer
and the victim. Some masks are equipped
with a one-way valve that allows the rescuer’s breaths to enter the victim’s
airway, but
prevents the victim’s expired
air from entering
the rescuer’s airway.
These masks also prevent
contact with vomitus and blood, which could pose an infection risk to the
rescuer. It takes practice to learn how to use these masks effectively to
provide ventilations.
USING A MASK:
a) Position yourself at the victim’s side. If you are a lone (single) rescuer, positioning yourself at the victim’s side will allow you to provide both ventilations and compressions without having to move.
b) Position the mask on the victim’s face. Masks are usually triangular in shape, and you will notice that the mask has a “pointy” end- this end goes over the bridge of the victim’s nose.
c) Seal the mask against the victim’s face. To do this, take the hand that is closest to the top of the victim’s head and place it along the edge of the mask. Some people find it easier to form a ‘C’ with their index finger and thumb and use these digits to grasp the mask around the base of the mouthpiece. With the thumb of your other hand, apply pressure along the bottom edge of the mask.
Then place the remaining fingers of your second hand along the bony edge of the jaw and lift the jaw upwards. Open the airway by performing a head-tilt chin-lift procedure. While you lift the jaw, ensure that you are sealing the mask all the way around the outside edge of the mask to obtain a good seal against the victim’s face.
d) Deliver air over 1 second, ensuring that the victim’s chest rises.
e) If the victim’s chest does not rise, reposition the mask and try to get a better seal. Remember, you should be lifting the victim’s jaw into the mask, rather than simply pushing the mask down onto the victim’s face.
f) Provide 2 ventilations over 1 second each with the mask after every 30 compressions.
g) If the victim has a pulse but is not breathing, provide rescue breathing by providing 1 breath every 5 to 6 seconds (10-12 breaths/minute). Check for a pulse every 2 minutes- if there is no pulse, start chest compressions along with ventilations at a rate of 30:2.






Comments
Post a Comment